Follow-up visits after a concussion: time to take preventive measures
March 13, 2024
Wayne Gretzky, Canadian ice hockey legend, is famous for the quote “Skate to where the puck is going, not where it has been.” Behind this saying is the thought of instead of chasing what’s already happened, try to get a step ahead. When it comes to concussions in sport, we are often reacting: reacting to an injury, reacting to a diagnosis, reacting to symptoms. But what if instead of reacting to everything in a concussion, we start going to where a concussion trends towards. That is, recovery and return to sport.
In health care, this is what is known as preventive measures. Parachute, a national organization dedicated to injury prevention in Canada, outlines in their concussion guidelines that athletes of all ages with an alleged concussion receive timely and appropriate care. While the focus is often on an initial diagnosis (which is most certainly the most important point of care), follow-up visits are regularly neglected.
READ MORE: Concussion guide for parents and caregivers
Returning children and youth to school and normal daily activities are the primary focus after the acute period of concussion, as school provides an educational environment, and both school and physical activities facilitate social development and mental well-being (Choe & Barlow, 2018). The goal is to increase cognitive or other activities to the point where no current symptoms are worsened or new symptoms are triggered, known as sub-symptom threshold cognitive activity (Master et al., 2012). If at any point symptoms worsen, then the individual is bumped back to the previous stage. This graded return strategy needs to be individualized to each child and youth’s specific needs, as this can help with resuming their pre-injury activities sooner (Kelleher et al., 2014). The overall management of pediatric concussion involves decisions around both return to school and return to activity, underscoring the importance of follow-up with a primary care provider after an initial concussion diagnosis.

Gaps in research
Follow-up visits are important for reassessment, management, and education, particularly for children and youth. Guidelines created by the Ontario Neurotrauma Foundation (ONF) specify that follow-up for a concussion (after the initial visit) should occur with a physician or nurse practitioner by 4 weeks after the initial injury (Velinkonja et al., 2017). However, we have identified in a review of the literature that children and youth are not consistently followed-up after an initial concussion diagnosis (Ramsay et al., 2023). Also, little can be concluded about the time from initial diagnosis to the first follow-up visit, and the factors that influence the number of follow-up visits. This is why we conducted the Pediatric Concussion in British Columbia (PCBC) Project, a population-based study using administrative data to identify the rates and the timing of the first follow-up visit for children after a diagnosis of concussion, factors associated with follow-up timing, and the impact of time to first follow-up on children’s health.
Key findings from the data
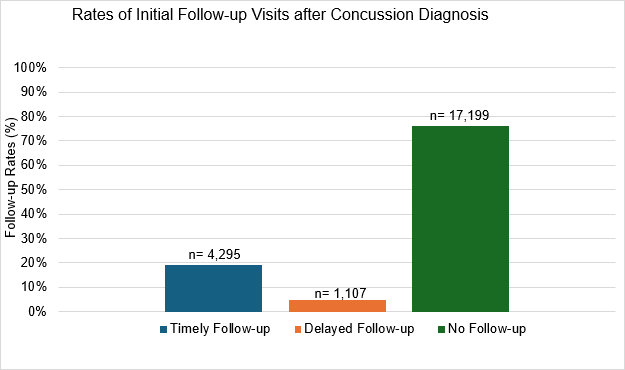
The study provides new insights into the rates and timing of follow-up visits, factors associated with the timing of the first follow-up visit, and the impact of that timing on residual health outcomes based on the administrative data from concussed children and youth aged 5 to 18 years in BC during 2016 and 2017. Linking datasets, a sample of 22,697 cases with an initial concussion diagnosis were identified. The 4 key findings from this study were:
- Follow-up visit rates are low for concussed children and youth in BC: less than 25% had any type of follow-up visit, of which only 19% had a timely follow-up visit.
- Among the children and youth who had a follow-up visit within 3 months of initial injury, 75% of cases attended a follow-up visit within 22 days, thus meeting the ONF recommended time of 28 days.
- Older age, living in a rural area, higher socioeconomic status, and seeing a specialist physician at the initial concussion diagnosis were associated with a timely first follow-up visit, but there may be other factors that contribute to timely follow-up.
- Concussed children and youth with a delayed follow-up visit were more likely to experience a health related to concussion compared to those with timely follow-up up to 12 months post-injury.
What to do next?
The results of the PCBC study identified the timing of the first follow-up visit after an initial concussion diagnosis and the health outcomes that happen. The findings from this study suggest that children and youth are not consistently followed-up after an initial concussion diagnosis. Historically, follow-up was either not required as part of concussion care or required only for patients with more severe brain injuries. However, given the potential for long-term health problems when follow-up is delayed, there needs to be a reframing of pediatric concussion care in Canada.
READ MORE: The 4 R’s: Steps to a Safe Recovery

To do this, our sporting bodies must enact concussion policies to protect athletes, so that we are not constantly reacting after every concussion. These policies include:
- training for sports personnel,
- concussion education for children and youth and their parents,
- return-to-play procedures,
- return-to-learn procedures, and
- medical clearance to return-to- sport.
Having an up-to-date concussion policy is a must. While this may protect some athletes from a concussion, it is important to remember that a concussion can still occur, and our research indicates that timely and ongoing care of a concussion will lead to better outcomes.
About the Author(s)
Scott Ramsay, PhD, RN is an assistant professor in the School of Nursing at the University of British Columbia and nurse clinician in neurology at BC Children’s Hospital. Scott uses population data methods to empirically document the access and use of health services on children with neurological conditions and its impact on health. He plays many sports, is avid bike rider and has coached ice hockey for over a decade. X: @scottramsay25
References
Choe, M., & Barlow, K. M. (2018). Pediatric traumatic brain injury and concussion. CONTINUUM, 24(1, Child Neurology), 300–311. https://doi.org/10.1212/CON.0000000000000569
Kelleher, E., Taylor-Linzey, E., Ferrigno, L., Bryson, J., & Kaminski, S. (2014). A community return-to-play mTBI clinic: Results of a pilot program and survey of high school athletes. Journal of Pediatric Surgery, 49(2), 341–344. https://doi.org/10.1016/j.jpedsurg.2013.10.016
Master, C. L., Gioia, G. A., Leddy, J. J., & Grady, M. F. (2012). Importance of ‘return-to- learn’ in pediatric and adolescent concussion. Pediatric Annals, 41(9), e160–e166. https://doi.org/10.3928/00904481-20120827-09
Parachute. (2017). Canadian guideline on concussion in sport. https://parachute.ca/en/professional- resource/concussion-collection/canadian- guideline-on-concussion-in-sport/
Ramsay, S., Dahinten, V.S., Ranger, M., & Babul, S. (2023). Follow-up visits after a concussion in the pediatric population: An integrative review. NeuroRehabillition, 52, 315–328. https://doi.org/10.3233/NRE-220216
Velikonja, D. O., Baldisera, T., Bauman, S., Davis, S., Di Salle, C., Freedman, M., Ouchterlony, D., Quon, D., Reed, N., Sims, K., Wilcock, R., Zemek, R., Kagan, C., Gargaro, J., Hansen, M., & Wiseman-Hakes, C. (2017). Standards for Post- concussion Care. Ontario Neurotrauma Foundation. https://concussionontario.org/wp-content/uploads/2017/06/ONF-Standards-for-Post- Concussion-Care-June-8-2017.pdf
The information presented in SIRC blogs and SIRCuit articles is accurate and reliable as of the date of publication. Developments that occur after the date of publication may impact the current accuracy of the information presented in a previously published blog or article.
