Beyond the ice: Former pro hockey player’s concussion struggles drive PhD mission for improved pediatric care for children and youth
January 15, 2024
In the halls of BC Children’s Hospital in Vancouver, Scott Ramsay witnessed a disconcerting pattern: children with concussions were being referred to the hospital too late, their symptoms already complex and challenging to manage. For Ramsay, a former professional hockey player turned nurse, this scene triggered a flashback to his own teenage years, marked by 4 concussions and the repercussions of post-traumatic concussion syndrome that followed.
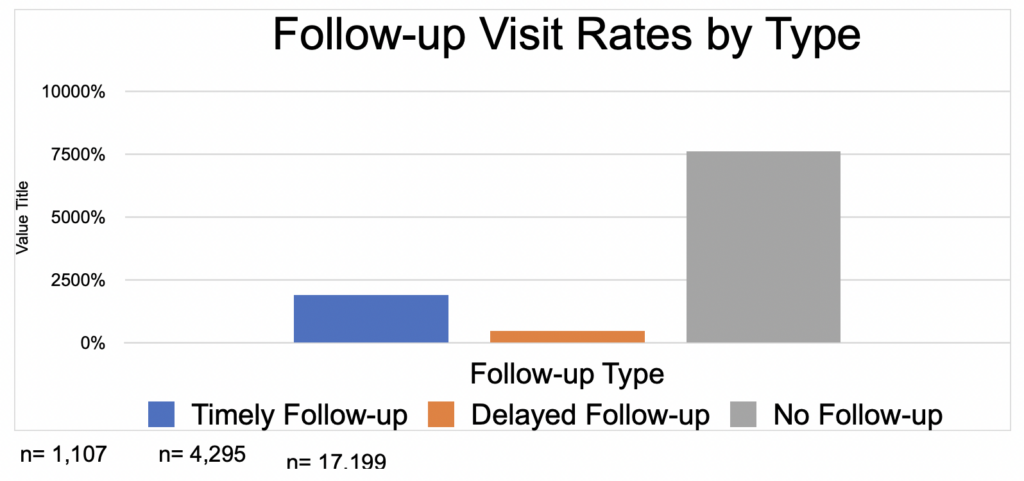
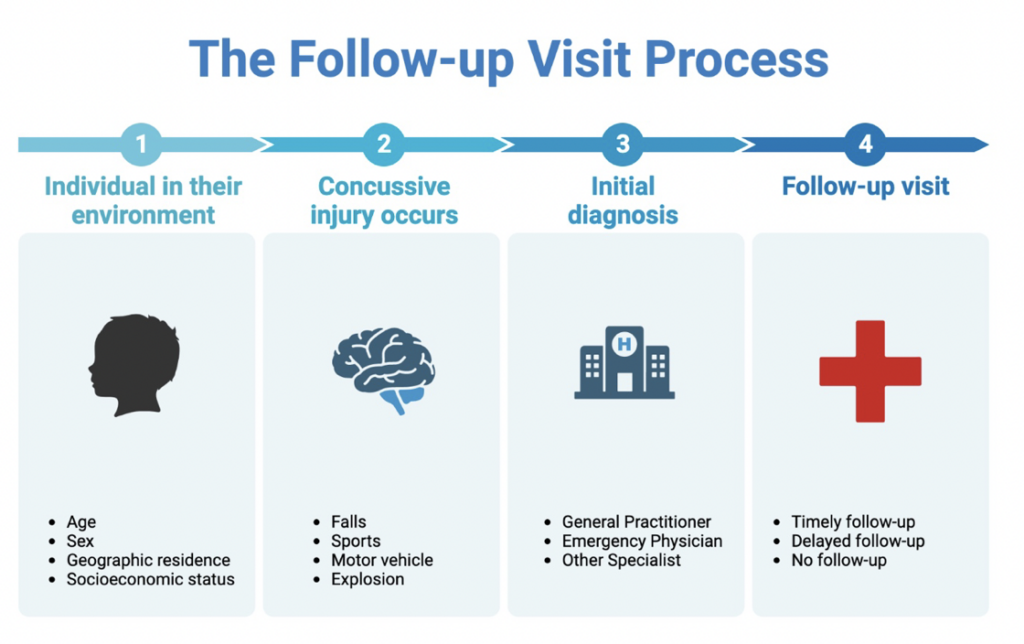
As Ramsay recently earned his Ph.D. in nursing from the University of British Columbia, his journey from the hockey rink to the hospital compelled him to take a closer look into an issue facing the health care system. The absence of educational interventions and post-concussion follow-ups for children in British Columbia. The issue caught his attention, prompting him to embark on a groundbreaking study for his dissertation involving just shy of 23,000 children and youth with concussions; a study now recognized as the largest of its kind in the province.
The results of his research shed light on a concerning reality: most concussed children and youth lack timely follow-up visits in BC, a finding that goes against the guidelines set by the Ontario Neurotrauma Foundation. Dr. Ramsay discovered that only 19 percent of young patients received a first follow-up within the recommended 4 weeks after diagnosis, leading to a higher incidence of persistent post-concussive symptoms.
Dr. Ramsay’s personal experiences, combined with the findings of his study, have fueled his commitment to advocating for change. His journey, from facing the challenges of post-concussion syndrome to becoming a dedicated nurse and researcher, highlights the critical need for improved education and awareness surrounding concussions in children.
Following in line with more education, Ramsay, along with SIRC’s extensive concussion in sport resources, provides an overview of what you need to know when it comes to concussions in children and youth.
What are the most common signs and symptoms of concussions in children?
Children often exhibit several common signs and symptoms when experiencing a concussion:
- Headache
- Dizziness
- Nausea and Vomiting
- Difficulty concentrating
- Sensitivity to light
- Ringing in the ears/Sensitivity to noise
- Behavioural Symptoms: inattention, irritability, heightened anxiety.
- Sleepiness
- Double or blurry vision
These symptoms serve as vital indicators for parents, coaches, and teachers to detect potential concussions in children early on.
Are there differences in signs and symptoms of concussions between children and adults?
Ramsay said due to the anatomical and physiological distinctions between children and adults, symptoms can sometimes be more intense in children.
- Anatomical differences: Children’s larger surface area and smaller bone structures can result in more pronounced injuries. This is crucial to understanding the severity of symptoms such as headaches and dizziness, which can be more intense in children due to their unique anatomical features.
- Cerebral blood flow: Variances in blood flow due to growth and development contribute to different symptom presentations.
- Hormonal factors: Differences in hormone levels, especially in the youth, may have associations with mental health issues like anxiety and depression.
How do you distinguish between a mild concussion and a more severe one in children?
Recognizing concussions in children poses unique challenges, Ramsay explains it starts with:
- A process of elimination: Ruling out other potential causes through a thorough medical history.
- A history examination: Investigating the circumstances leading up to the injury and understanding the symptoms.
- Reporting challenges: Children may not always communicate incidents of head injury, making accurate diagnosis challenging.
Ramsay also emphasized the importance of listening to children, highlighting the difficulty in cases where children may not readily communicate their head injuries. This insight underscores the complexity of diagnosing concussions in children and the need for careful consideration of the circumstances surrounding the injury.
READ MORE: Concussion guide for parents and caregivers
What immediate steps or first aid measures should be taken if a child is suspected of having a concussion?
- Removal from activity: Taking the child out of the sport or event immediately.
- Get medical attention: the child should not be left alone and should be seen by a medical health professional as soon as possible that day.
- Check for red flag symptoms: seizures, posturing, vomiting, and unequal pupils.
- Urgent Medical Attention: Contacting 911 if red flag symptoms are present or the child loses consciousness.
This immediate response is crucial in preventing further harm and initiating the necessary steps for proper diagnosis and care.
How long do symptoms of a concussion potentially last? Are there any factors that can influence recovery time?
- The signs and symptoms of a concussion often last for 1 to 4 weeks but may last longer.
- In some cases, children may take many weeks or months to heal.
- Factors influencing recovery:
- Prior concussion history (If your child has had a concussion before, they may take longer to heal)
- Pre-existing conditions, and external factors like stress can impact recovery time.
READ MORE: The 4 R’s: Steps to a Safe Recovery
What role do cognitive and physical rest play in the recovery process for child with a concussion?
- Initial Rest Period: Recommending rest for 24-48 hours, followed by gradual reintegration into daily activities.
- Cognitive rest: The child may find it hard to concentrate in class, may get a worsening headache, or feel sick to their stomach. If so, the child should stay home if being in class makes their symptoms worse. Once they feel better, they can try going back to school part-time (half day) and then a full day.
- Return-to-Sport or physical activity:
- Stage 1: Symptom-limiting activities: After an initial short period of rest of 24 to 48 hours, light physical activity can begin, as long as these don’t worsen symptoms.
- Stage 2: Light aerobic activity: Such as walking or stationary cycling, for 10 to 15 minutes. The duration and intensity of the aerobic exercise can be gradually increased over time if symptoms don’t worsen, and no new symptoms appear during the exercise or in the hours that follow. No resistance training or other heavy lifting.
- Stage 3: Individual sport-specific exercise with no contact: Activities such as skating, running, or throwing can begin for 20 to 30 minutes. There should be no body contact or other jarring motions, such as high-speed stops or hitting a ball with a bat. No resistance training.
Medical clearance and a full return to school are required to progress to Step 4
-
- Stage 4: Begin training drills with no contact: Add in more challenging drills like passing drills. There should be no impact activities (no checking, no heading the ball, etc.). Start to add in progressive resistance training.
- Stage 5: Full contact practice following clearance by a doctor.
- Stage 6: Return to Sport
MORE INFORMATION: Living Guideline Return to Activity/Sports Protocol
What are the potential long-term effects of repeated concussions in children?
Delving into the long-term effects, Ramsay pointed out the limited evidence regarding the precise outcomes of repeated concussions in children. Drawing on studies in adults, he highlighted cognitive impairments, decreased quality of life, and psychosocial challenges as potential consequences.
While acknowledging the gaps in current knowledge, Ramsay’s insight and research provide a foundation for understanding the potential risks associated with repeated concussions in the pediatric population.
Fact or Myth: Children and youth who sustain a concussion have a higher risk of experiencing mental health issues than children and youth who experience other types of injuries. By Dr. Roger Zemek, MD, pediatric emergency physician at Children’s Hospital of Ontario (CHEO).
How would you go about educating parents, coaches, teachers, about the signs and symptoms of concussions, to ensure early detection and appropriate care?
Ramsay advocates for active listening and taking children’s symptoms seriously. He underscored the importance of open conversations to reduce stigma and creating a supportive environment for reporting head injuries. By emphasizing that there’s no shame in admitting to a head injury, Ramsay encourages a cultural shift toward recognizing and addressing concussions in children.
His approach to education involves instilling a sense of responsibility among parents, coaches, and teachers to prioritize the well-being of children and actively engage in conversations that contribute to early detection and appropriate care.
Want to learn more about sport-related concussions and what education programs and tools are available. Find out more through this comprehensive list of programs put together by SIRC and their partners.
In your experience, what are some challenges in recognizing and managing concussions in children and how can these challenges be addressed?
Ramsay acknowledged the challenges in recognizing and managing concussions in children, pinpointing the underreporting of concussions as a significant hurdle. He stressed the importance of establishing reporting mechanisms in sports settings and encouraged seeking care from qualified healthcare professionals for accurate diagnosis and management.
Why is it important to talk about this specific topic like signs and symptoms and kids based on your experience? Why should we be talking about this?
Highlighting the significance of the conversation, Ramsay emphasized the role of timely care in improving the likelihood of a child returning to normal life sooner. He stressed the importance of proper management throughout the recovery trajectory to minimize post-concussion symptoms.
Ramsay underscored that talking about the signs and symptoms of concussions in children is not just about raising awareness; it’s about fostering an environment where early detection, appropriate care, and continuous support are prioritized for the well-being of the younger population.
READ MORE: Key topics in concussion research
About the Author(s)
Dr. Scott Ramsay, Ph.D., is an assistant professor in the School of Nursing at the University of British Columbia and Nurse Clinician in the Neurological Care Centre at BC Children’s Hospital. Dr. Ramsay focuses on the health care services for children and youth with neurological conditions, and the study of factors impeding care. He is interested in the integration of multidisciplinary care in the delivery of care for individuals with a traumatic brain injury. Prior to becoming a nurse and researcher, Scott was a high-level hockey player, where he suffered 5 concussions and post-concussion syndrome. He utilizes his unique perspective as a brain injury survivor, clinician, and researcher to collaborate with patients, clinicians, policymakers, and researchers, given his multiple roles in the care of children and youth with a brain injury in British Columbia.
Paula Baker, M.Sc., is the managing editor at SIRC. In this role, she draws on her 20 years of experience as a journalist, and as a former exercise physiologist, to bring sport research, knowledge, and the occasional human-interest story, to our readers.
The information presented in SIRC blogs and SIRCuit articles is accurate and reliable as of the date of publication. Developments that occur after the date of publication may impact the current accuracy of the information presented in a previously published blog or article.
