Highlights
- Our bodies experience cold as a physiological stressor, meaning that one’s body must work hard to keep itself in thermal balance
- It is important for athletes and coaches to be aware of ways to mitigate the risks of cold exposure, which can include tissue injury and diminished cardiovascular capacity
- This article summarizes the research on cold exposure as it relates to exercise and presents strategies to promote safe participation, training and competition in outdoor sport activities during the winter months
- This article has a sibling article on training and competing in extreme heat
Let’s face it, being an athlete that trains outdoors during the winter can be stressful. Cold hands, runny nose, dry eyes, burning lungs, and wearing too little or too much are all realities athletes in Canada face throughout the winter. Luckily, our understanding of how humans can exercise safely and effectively in cold weather has improved. This article summarizes the research on human responses to cold exposure and presents evidence-informed strategies to promote safe participation, training and competition in outdoor sport activities during the winter months.
While there are different types of cold that athletes and outdoor enthusiasts may be exposed to, including cold air and cold water, this article will focus on cold air (because most decisions we make regarding winter outdoor physical activity and exercise are not in water, thank goodness). If readers are interested in understanding more about the effects of swimming in very cold water please see Tipton et al. (Tipton & Bradford, 2014) or are interested winter swimming challenges see Manolis et al. (Manolis et al., 2019).
Science of human responses to cold exposure
At 30 degrees Celsius, humans perceive water as cold (Smith & Hanna, 1975), and in a semi-nude state your body perceives 28.5 degrees Celsius air as cold (Kingma et al., 2012). In general, cold water or cold air is called a “physiological stressor,” which just means your body recognizes cold as something it needs to accommodate to stay in balance (body equilibrium). These mechanisms for cold stress (just like heat stress) are tightly regulated and every minute of the day your body is trying to ensure you are in “thermal balance.”
As it relates to cold environments thermal balance is the functional way to maintain comfort, overall body temperature and protect your core temperature. This is because unless extreme cold or prolonged exposure to cold overwhelms your ability to maintain your core temperature, thermal balance is your main consideration while being active in cold environments. To maintain thermal balance you are constantly balancing “heat loss factors” with “heat gain factors.”
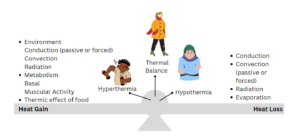
Thermal Balance is a product of heat loss and heat gain factors. On the heat loss side of Figure 1: conduction is the heat exchange between the skin or clothed parts of your body in direct contact with colder surrounding surfaces (for example, an ungloved handing touching a cold door handle or standing on snow). Convection can be natural (air movement on skin which can be between a base layer of clothing or unclothed skin such as your face) or forced (where your body is moving in motion throughout air or water) both of which cause heat to be transferred from the body to the air. Radiation is the heat energy transfer from your body to the surrounding environment.
On the heat gain side of Figure 1: radiation is the effect that the sun has on transferring energy to your body. Conduction can be adding heat to your body if the thing you are touching is warmer than your tissue temperature (think about the heat packs that you add to your gloves on cold days). Convection can cause heat gain when air warmer than your skin (for example, think about walking into a warm ski lodge after skiing in the winter). Metabolism is the energy produced from body fuels (fat stores, sugars in your body) for resting metabolism (all the energy it takes to keep your body alive) and muscular activity (extra energy being made to allow you to complete whatever physical activity you are doing). The thermic effect of food refers to the energy required for digestion, which does add some excess heat production (this is why you feel hot after a really large meal).
Core temperature is the temperature of your trunk and head (Lenhardt & Sessler, 2006) and your normal core temperature is about 37 degrees Celsius (Kurz, 2008), though your body core temperature can vary by up to 1 degree Celsius over the course of a 24 hour period (Kurz, 2008).
Mean body temperature on the other hand is the combination of your core temperature and your extremities, which are usually 2 to 4 degrees cooler than your core (Sessler & Todd, 2000). Your body will defend core temperature via many mechanisms in cold environments but if it cannot then accidental hypothermia risk increases.
Accidental hypothermia occurs when there is an involuntary drop in core temperatures < 35 degrees Celsius, leading to serious medical consequences (Castellani et al., 2021). Accidental hypothermia can occur in athletes exercising in a variety of air temperatures, especially if a combination of environmental “wet or windy” conditions are present, the individual has reduced exercise intensity due to fatigue or low blood sugar levels (Procter et al., 2018) or lack of adequate insulative wind/water proof clothing (Burtscher et al., 2012).
One less recognized factor that can affect body temperature is sweat either on the skin or in base layer clothing (Morrissey & Rossi, 2013). Getting sweaty due to inappropriate type and amounts of clothing while exercising vigorously can lead to extreme thermal discomfort (feelings of skin clamminess and coolness and overall perceptions of feeling cold) (Morrissey & Rossi, 2013) as well as a potential reduction in core temperature (Castellani et al., 2006). This is because sweaty skin at 5 degrees Celsius anywhere on your body is at least 10 degrees Celsius colder than dry skin in air that is 5 degrees Celsius (Pugh, 1967).
Exposed skin in cold environments can be both physiologically challenging to your body as well cause injury. Frostbite is an injury to the skin (particularly exposed skin) most often seen on hands, feet, nose and ears where frostbite risk is accelerated by wind speed, wetness of the skin and touching cold materials such as metal and snow. Early symptoms in frostbite are numbness, white or yellow skin, or waxy looking skin (Castellani et al., 2021). More severe frostbite is associated with the tissue feeling “cool to touch” or tissue feeling like a “block of wood”(Castellani et al., 2021). Current time estimates for frostbite injury show that 15 km/hr wind speed at air temperatures of –20 degrees Celsius can lead to significant tissue injury in 10 to 30 minutes (Castellani et al., 2021).
 In addition, exposing any skin on your body to cold environments can lead to a host of additional adjustments to ensure your overall body temperature is maintained, and some of these adjustments influence your comfort and ability to exercise. The wide range of responses to exposed skin in cold environments is due to the fact our body has thermoreceptors (nerve endings that sense temperature) everywhere on our body. They are there to provide immediate feedback to your brain to ensure your core temperature and overall body temperature are maintained, however, the responses can alter your ability to exercise. For example, – 20 degrees Celsius air blown across a person’s face exercising at a moderate intensity can increase oxygen cost (you work harder (Stroud, 1991)) and your VO2max has been shown to be significantly lower in -18 degree Celsius air compared to warm environments (Stensrud et al., 2007). Furthermore, the thermoreceptors in your face can affect your lung function, constricting your lungs, even if you are breathing warm air (Koskela & Tukiainen, 1995).
In addition, exposing any skin on your body to cold environments can lead to a host of additional adjustments to ensure your overall body temperature is maintained, and some of these adjustments influence your comfort and ability to exercise. The wide range of responses to exposed skin in cold environments is due to the fact our body has thermoreceptors (nerve endings that sense temperature) everywhere on our body. They are there to provide immediate feedback to your brain to ensure your core temperature and overall body temperature are maintained, however, the responses can alter your ability to exercise. For example, – 20 degrees Celsius air blown across a person’s face exercising at a moderate intensity can increase oxygen cost (you work harder (Stroud, 1991)) and your VO2max has been shown to be significantly lower in -18 degree Celsius air compared to warm environments (Stensrud et al., 2007). Furthermore, the thermoreceptors in your face can affect your lung function, constricting your lungs, even if you are breathing warm air (Koskela & Tukiainen, 1995).
Interestingly, your respiratory system (which includes your sinuses, mouth, throat and lungs) is like your skin. Even though it is inside your body, it is considered directly exposed to the environment because there is no barrier to the surrounding environment. Thus, your lungs, like your skin, are vulnerable to the cold air conditions, and breathing cold air can trigger thermoreceptors in the upper respiratory system, which affects your cardiovascular response to exercise (Heindl et al., 2004).
Our research has shown that when you exercise at a hard intensity, your lungs do a good job at warming and humidifying air in temperatures warmer than – 15 degrees Celsius, but temperatures colder than –15 degrees Celsius affect the lining of your lungs, leading to constriction and respiratory symptoms (cough, burning or sore throat, wheeze, more mucous) both during and after exercise (Kennedy et al., 2019). Exercising in very cold air leads to what is called respiratory evaporative heat loss (that feeling that your chest is cold inside) (McFadden Jr et al., 1999) and your body needs more water to humidify air in cold air (especially if you are breathing heavily) (Koskela, 2007), which means your lungs work much harder in cold air than warm air to stay functional.
From a thermal comfort standpoint, we know that your body early in the winter perceives cold air as a greater stressor than later in the winter (Van Ooijen et al., 2004). This can be an advantage in situations such as the Canadian Men’s Soccer Team qualifying run for World Cup 2022. In these cold games, for example in Edmonton on 16 November 2021 where the air temperature was – 9 degrees Celsius, the Canadian team likely perceived cold stress as lower due to their habitual exposure to cold over years compared to their Central American opponents. Although significantly understudied compared to heat acclimation, leading experts in the field provide clear evidence that 10 days of cold exposure can alter perception and reduce cold defence mechanisms (Yurkevicius et al., 2022).
Applying the science of cold exposure to exercise and sport
 Remember from Figure 1 that there are several different ways we can lose heat, and these potential losses of heat are all to some degree affected by how much the body is exposed to the environment. Thus, adding insulative clothing helps provide resistance to cold stress, and can do so very effectively, especially if you are exercising in sub-zero temperatures. The science of insulative clothing is based on “clo” units where 1 clo is equal to the air trapped between the skin and the layer of clothing needed to keep someone comfortable at rest in 21 degrees Celsius (Gagge et al., 1941). However, since the original research was conducted in the 1940s, better “insulative materials” have been developed that are more breathable and also wind and water proof, meaning we can extend the range of cold temperatures we can be active in while better maintaining thermal comfort (Liu et al., 2022).
Remember from Figure 1 that there are several different ways we can lose heat, and these potential losses of heat are all to some degree affected by how much the body is exposed to the environment. Thus, adding insulative clothing helps provide resistance to cold stress, and can do so very effectively, especially if you are exercising in sub-zero temperatures. The science of insulative clothing is based on “clo” units where 1 clo is equal to the air trapped between the skin and the layer of clothing needed to keep someone comfortable at rest in 21 degrees Celsius (Gagge et al., 1941). However, since the original research was conducted in the 1940s, better “insulative materials” have been developed that are more breathable and also wind and water proof, meaning we can extend the range of cold temperatures we can be active in while better maintaining thermal comfort (Liu et al., 2022).
The other good news is that our bodies are between 20 and 30 % efficient, meaning we produce a lot of heat while exerting energy to exercise (Whipp & Wasserman, 1969). So, if we wear enough proper insulative clothing, we can achieve thermal balance quite easily. The multi-layer approach is still highly recommended (base wicking layer, insulative mid-layer and the breathable but windproof outer-layer) because it allows for thermal balance to be readily controlled (Morrissey & Rossi, 2013).
However, it is important to remember sweaty skin is the real culprit with regard to discomfort and thermoregulation, so choosing the right ensemble of clothing really matters, to ensure that sweat does not accumulate on skin, in your base layer, or increase condensation within the outer shell (Huang, 2016). An outer shell that has a hydrophilic layer (attracts moisture to vent) is the best option for reducing condensation. However, in addition, wearing looser clothing allows for greater water vapour transmission through the base layer (reduced water on skin) and maintains air layers between layers (which improves heat retention). Thus, choosing the correct combination of technical clothing layers that maximize wicking offers thermal resistance (warmth), are highly breathable but wind proof as well as looser will ensure good cold weather thermal management (Morrissey & Rossi, 2013; Tang et al., 2014).
Our recent research looking at exercise in – 15 degrees Celsius found that despite tissue temperature throughout the body decreasing, warm up exercise intensities were sufficient to maintain thermal comfort. The participants wore a base layer, a thin Lycra® mid layer and technical warm up suit (Gore-Tex Infinium®) and an early conclusion from this study would be that “starting cold” will ensure you don’t overheat during the main part of your workout.
Covering your skin as much as possible will have some obvious benefits in reducing frostbite risk, while also reducing thermoreceptor strain. This includes covering your cheeks, forehead, nose and neck, especially in windy conditions (Mäkinen et al., 2000), even in conditions that Canadians might not consider “that cold” (-5 and -10 degrees Celsius). Covering your mouth and nostrils via some type of mask or “heat and moisture exchanger” device (for example, AirTrim®), certainly has benefits in reducing strain on the respiratory system and reducing the chances of having cold induced shortness of breath or asthma like attack (narrowing of the airways in your lungs) (Frischhut et al., 2020). Interestingly, some recent research has also found that maintaining temperature in your nostrils ensures you have preserved your ability to fight off inhaled viruses, which is one more reason to wear a mask (Huang et al., 2022).
Concluding thoughts on safety and performance in cold
If you are parent, coach or involved in youth sport organization, remember that prevention matters. Canadians often have a “tough it out” attitude to cold weather and we likely expose ourselves to too much cold air for our own good. With that being said, there is no clear indication of what is considered “too cold” in Canada, and most sports have some cold weather policies that are based on old evidence or just expert opinion. The emerging science would indicate that if we can reduce those severe exposures on an annual basis, we will reduce the incidence of asthma and exercise induced asthmatic conditions, catastrophic medical situations and cold weather deaths. Given that I consistently advocate for safer cold weather training and competitions environments I will leave you with these thoughts:
- Spend your money on good quality technical gear for your body, head and neck regions
- At -15 degrees Celsius and colder, consider staying indoors for a workout, or modify the workout to reduce exposure to cold
- Keep track of your own and your athlete’s respiratory symptoms. If they report any of the following symptoms in the 24 hours after a cold weather workout or competition or game, you should think about reducing continued cold exposure until the symptoms resolve:
- Uncontrolled cough, cough so bad you feel like you will vomit
- Deep breath or temperature change that makes you sensitive to cough
- Wheezing
- Chest tightness (band around my chest)
- Trouble breathing (feel short of breath)
- Chest pain (like lungs hurt)
- Excessive mucus in lungs or nose
- Tickle in your throat, sore throat, persistent dry throat
- Hoarse voice (makes it hard to talk), raspy voice
- Taste of blood
- If you engage in activities such as cross-country skiing or running outdoors in the winter, you have a greater risk of stressing your lungs. This is because these activities have you breathing heavily for a prolonged period of time (called high ventilation activities) and breathing large amounts of cold dry air is a known risk factor for lung dysfunction (Carlsen, 2012)
- Ensure you follow up with your health care provider to ensure your lung health is maintained, especially if you have any significant bouts of respiratory symptoms or feel short of breath during or in the 30 minutes after your cold weather exercise bout
- If you are middle aged and regularly exercise in cold, know that there is increased mortality in winter months due to Sudden Cardiac Death (Ryti et al., 2017) that is attributed to cold weather exposure (so make smart choices on how hard you exercise and if you should exercise outside on cold days)
- Drinking more water in the cold winter months is important to your hydration status and your lung health. Remember you can lose up to 100 millilitres of water per hour in – 4 degree Celsius air due to heavy breathing exercise in cold air and this needs to be replaced in addition to your normal water losses (Freund & Sawka, 1996)